

General management and drug therapy Acute adrenal insufficiency

Then see General management and drug therapy section below. See appendix 1 of the GGC guideline on Suspected Iatrogenic Adrenal Insufficiency. Establish venous access and draw blood for U&Es, glucose, cortisol and ACTH (adrenocorticotropic hormone).Diagnostic measures should never postpone treatment and if adrenal crisis is suspected, treatment should be initiated without delay.If patient has suspected acute adrenal insufficiency: It complements the GGC guideline on Suspected Iatrogenic Adrenal Insufficiency, which describes the assessment of adrenal function in patients on glucocorticoid for a non-endocrine condition. This guideline advises on the general management of adrenal insufficiency in an acute situation and the diagnosis of it in the non-acute. suppression of hypothalamic-pituitary axis by various factors).

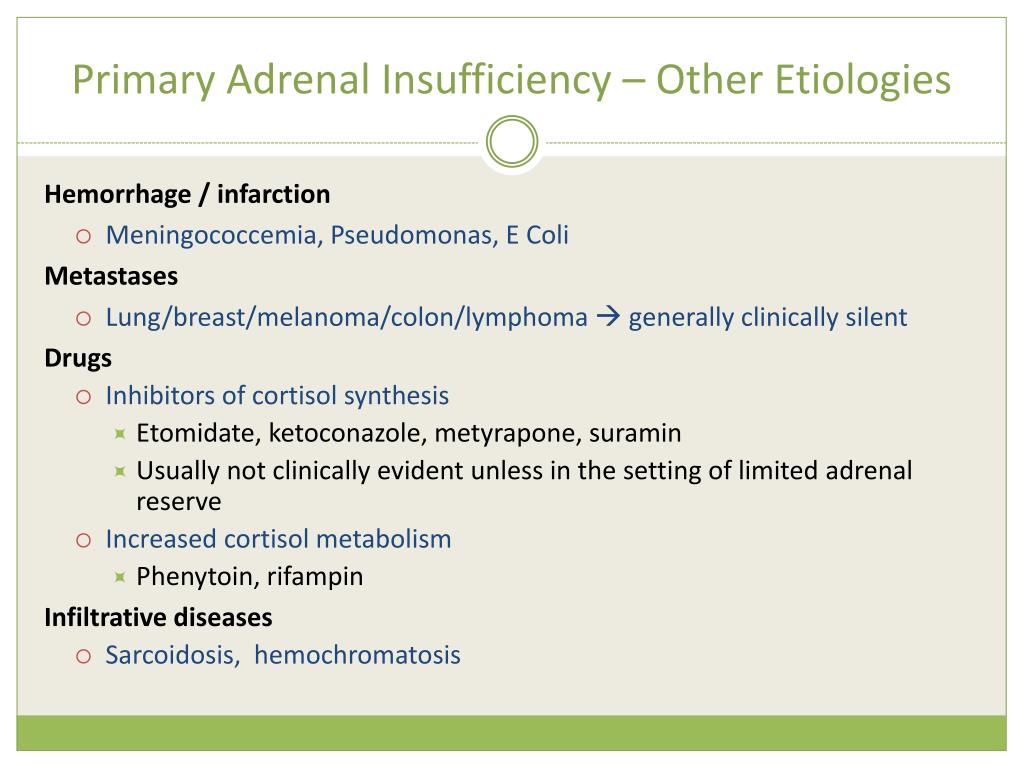
there is structural damage to the gland) or secondary (e.g. When there is insufficiency it can either be primary (e.g. The adrenal cortex is responsible for producing glucocorticoids, mineralocorticoids and androgens.
This can happen if the pituitary gland is damaged by things like a tumour or surgery. When the pituitary gland doesn't make enough ACTH, the adrenal glands won't make enough cortisol. The signal is a hormone that the pituitary gland makes, called ACTH. Normally it sends a signal to the adrenal glands to make more cortisol. The problem starts with the pituitary gland. It helps break down sugar and fat for energy. Secondary adrenal insufficiency means that your adrenal glands don't make enough of a hormone called cortisol. They make hormones that affect almost every organ in your body. Your adrenal glands sit on top of your kidneys.


 0 kommentar(er)
0 kommentar(er)
